The third UN Millennium Development Goal seeks to ensure a healthy life “for all”. Using height inequality as an indicator, this column shows that the introduction of public health insurance schemes over the last 150 years substantially reduced health inequality. However, a variety of outcome measures are needed to monitor health inequality in order to devise policies that can reduce it.
The third UN Millennium Development Goal seeks to ensure a healthy life “for all”, i.e. including the lower income groups of populations. However, if you were born into a poor family in a low-income country, your life will typically be shorter and less healthy than it could be, so a major policy concern is to reduce health inequality in the world. One potential instrument is the introduction of universal health insurance. Several studies have found that insurance expansions of the recent past have been followed by improvements in several health outcomes including infant and child mortality, as Currie and Gruber (1996) document after the implementation of Medicaid in the US. Goodman-Bacon (2021) compares birth cohorts before and after the introduction of Medicaid in different US states and finds that children eligible for Medicaid in their early years are significantly healthier and financially better off as adults. A person’s health during childhood is significantly influenced by their parents’ actions. And these actions are guided by medical interventions such as dietary advice, access to vaccinations, regular health screenings, and treatments for specific conditions. These factors have a crucial impact on a person’s health later in life. Furthermore, health insurance gives people more financial stability, which reduces stress from going bankrupt and improves wellbeing (Haushofer et al. 2020).
However, the effect of universal health insurance, or ‘universal healthcare’, on health inequalities in the long run has not been studied yet. In a recent paper (Baten et al. 2024), we assess progress, and also periods of stagnation, in health inequality. In particular, we consider the prominent instrument of UHC.
The origins of social health insurance
The first health insurance scheme was implemented in Germany in 1883. Germany was quickly followed in the 1880s by other Western European countries such as the Habsburg Empire, which included modern-day Austria, the Czech Republic, Hungary, and Slovakia. Many countries developed health insurance programmes in the decades that followed, particularly in the 1940s.
The expansion of health insurance to larger segments of the population was crucial to expand access to medical care, and potentially improve human health in the 19th and 20th centuries. Driva et al. (2017) document that the expansion of health insurance in Germany reduced mortality. Following Bismarck’s lead on expanding the number of people insured in Germany, the proliferation of state-funded health insurance in Denmark, Belgium, Norway, and the UK significantly reduced the costs of access to health technologies.
Over the last 150 years, health insurance has been expanded to larger parts of the population, starting from workers, via elderly insurance, to the whole population. Today, we talk about universal healthcare, which the WHO defines as access to the national health system for (almost) all people living in the country. This system could be publicly and/or privately funded. Taken as the basis of our measurement, as of 2010, we can find evidence of 43 countries around the world having formally introduced UHC that covers more than 90% of their population.
Addressing health inequality via social insurance
Insurance minimises the risk of unexpected medical costs that individuals or households would instead have to bear (Meghir et al. 2015). When costs are unaffordable, people forego healthcare, which can have negative consequences for their health. In a recent report, the WHO Health Observatory shows a staggering progress of health inequalities in the Estonian population, with figures indicating spikes in premature deaths from health disparities among those in lower income groups. It concludes that unequal health outcomes among individuals are rooted in factors such as socioeconomic status, education, and living standards. Increasing health insurance coverage would lead to large utility gains for households through the reduction of uncertainty and variable health-related expenditures (Einav and Finkelstein 2018). Of particular interest is the effect of insurance extensions on individuals who otherwise would have undergone healthcare difficulties. In addition to improving health for the whole population, health insurance expansion is likely to influence health inequalities by progressively including segments of the population that are more in need. Therefore, improving the health of those with the worst health conditions reduces health disparities in a population if the marginal contribution of healthcare access and utilisation to one’s health is larger at lower levels of the health status distribution.
In our paper (Baten et al. 2024), we examine whether expanded access to health insurance has historically reduced height inequality by promoting body growth in poorer households in particular, because greater equality implies that children of poorer households could receive more critical resources (i.e. nutritional quality and healthcare), and therefore increase the height of their children. Height inequality is a widely used and well-established anthropometric measure of health inequality, but it has never been used for assessing the effect of health insurance. Most insurance expansions across countries took place at a time when there was little access to health indicators to measure the effects of the expansions, which limited the analysis of insurance on well-defined health measures such as mortality (Bauernschuster et al. 2020). This measure is also very sensitive to improvements in standards of living and early-life health investments. As a practical advantage, once adulthood has been reached, height is stable (up to around the age of 50), hence one adult survey allows us to study height inequality for several birth decades (after studying survivor bias). In sum, socioeconomic circumstances can influence individual heights, and therefore height disparities in a population.
The extent of health inequality globally and within specific regions
We document rising height inequality between different world regions despite similar starting s in the birth decades of around 1870-1880, before the Bismarckian social insurance system was introduced in Germany. World regions with early health insurance systems tended to have lower height inequality thereafter. The 19th century was also a period, after an initial worsening before WWI, of substantial achievements in improving health conditions across many societies and in reducing inequalities in health (Deaton 2003, 2013). After the birth decade of the 1920s (i.e. 1920-1929) in particular, we observe a reduction in the height Gini indicator. For Europe in particular, inequality began to fall after the birth decade of the 1920s. In Africa, on the other hand, height inequalities increased between the birth decades of the 1930s and 1960s. We observe that during the birth decade of the 2000s, inequality levels were highest in South America and Africa, where universal healthcare tended to be less generally available.
Historical expansion – but still lacking universal health coverage
In Figure 1, we demonstrate that countries with universal health coverage have lower height inequality, with a difference of 6.3 Gini points for the entire sample period starting from the 1810s (left panel), and 10.9 Gini points for the 2000-2009 birth decade (right panel). In our IV regression analysis, we find that within-country height inequality declined after insurance expansions towards near-universal coverage. Theoretical explanations could be that social insurance provide improved access to information gatekeepers, such as physicians, and influenced individuals’ behaviour and health utilisation through preventive and curative care (Freeman et al. 2008). Insurance expansion can be important in promoting the uptake of preventable behaviours. People are more likely to adopt highly valuable health behaviours when they receive information from a source they trust, such as healthcare providers or even a health professional in their own family (Persson et al. 2019). Insurance could also reduce the impact of cognitive biases that lead to negative behavioural risks (Baicker et al. 2015) and the underuse of health care. Such effects are especially important among unskilled, low-income, and near-elderly adults, who are otherwise uninsured (Finkelstein et al., 2012).
Figure 1 Differences in height inequality by universal health coverage
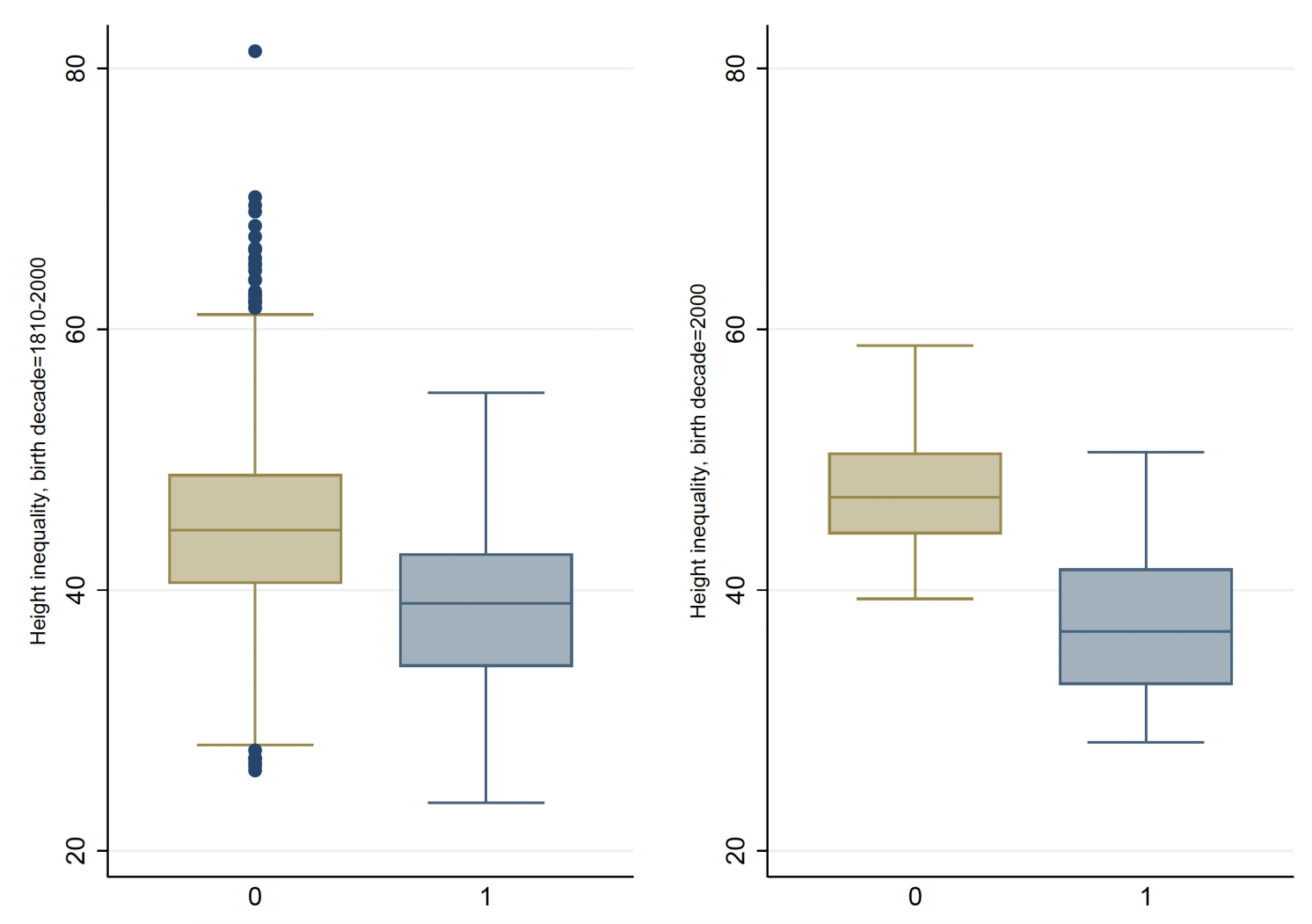
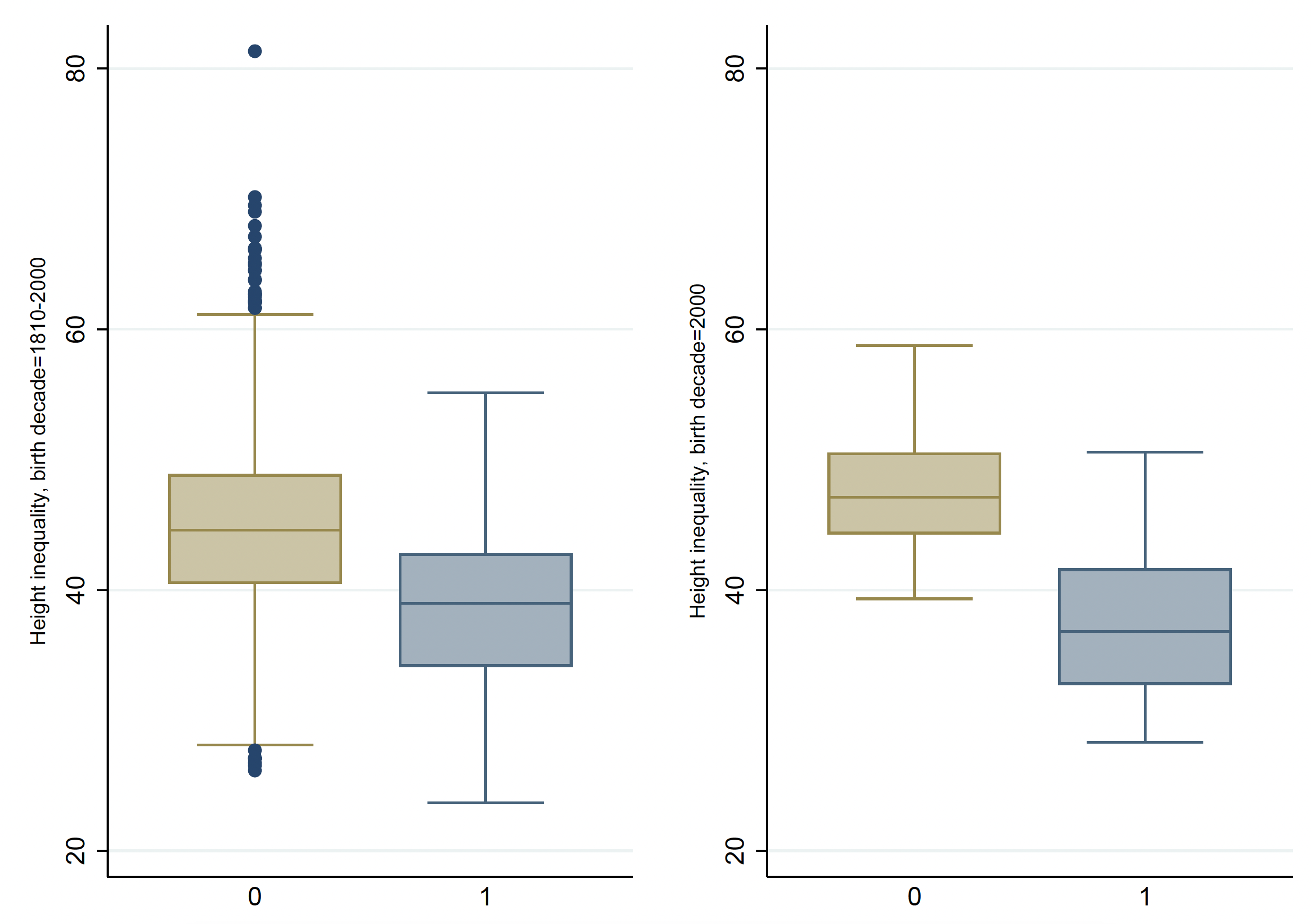
Notes: The figure shows the difference in height inequality by countries with (=1) and without (=0) UHC, for the whole period 1810–2000 on the left, and for the birth decade 2000 on the right. Height inequality is measured as the Gini coefficient.
The way forward/policy advice
Our results suggest that health insurance expansions have contributed to reducing health inequality. Pursuing substantial universal health insurance coverage improves access to health and represents a pathway to reducing health inequality. Looking at height inequality suggests that underserved and neglected populations are more likely to benefit from insurance expansions. However, egalitarian health policies need to be monitored carefully. In order to reach the third Millennium Development Goal of “health for all”, a variety of outcome measures, including height inequality and several other indicators, need to be taken into account, as we have done in our study.
Source : VOXeu