The COVID-19 pandemic was a disaster. It led to at least 6 million deaths, caused tremendous economic and social disruption, and unwound decades of development gains in vulnerable lower-income countries.
While health care workers played a critical role in saving people’s lives, they faced a much higher risk of infection and death, particularly in the early stages of the pandemic. This is largely because they were not protected by sufficient infection prevention and control (IPC) protocols –basic measures that should be present in every health facility which led to more infections and deaths among both health care workers and their patients.
Until now, the economic costs of these largely preventable infections to the health care system and to national economies have not been quantitatively estimated.
The economic costs of COVID infections in health care workers
A new joint study by the World Bank and Resolve to Save Lives conducted across four countries in Africa and South America shines a light on this overlooked but major systems failure. The study provides a framework for better understanding the economic burden and more accurately estimating the direct and indirect cost (medical and non-medical cost, productivity loss) of COVID-19 infections among health care workers and secondary infections transmitted by infected health care workers, as well as cost related to the disruption of essential services due to compromised health workforce.
There were three key takeaways from this study.
1. Preventable COVID-19 infections in health care workers had enormous economic costs
In the pandemic’s first year, COVID-19 infections and deaths among health care workers posed a substantial economic burden to society, with regions that could least afford to lose health care workers to illness or death being the most heavily impacted.
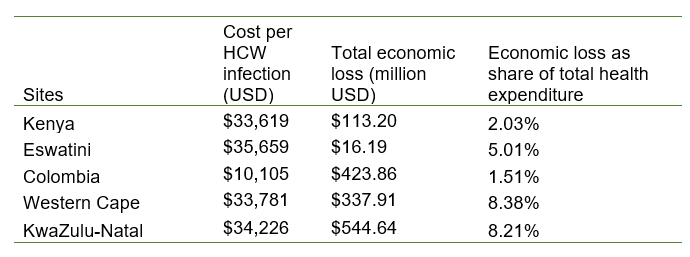
Taking into account primary infections and deaths among health care workers, as well as the impact from secondary infections and service disruption, the study determined that the overall economic burden of health care worker COVID-19 infections ranged from $16.2 million in Eswatini to $544.6 million in KwaZulu-Natal Province of South Africa. The cost per infection was similar in four of the five sites studied, around $35,000; in Colombia, the country’s relatively robust health system contributed to a much lower cost per infection of about $10,000. When compared to total health expenditures, the economic burden is substantial, ranging from 1.5% in Colombia to 8.4% in the Western Cape province of South Africa (Table 1).
Table 1. Cost of SARS-CoV-2 infection among HCWs
2. Infected health care workers had a huge and far-reaching impact
The cost from secondary infections and service disruption often outweighed the cost from primary COVID-19 infection among health care workers. Health care workers who are sick and unable to work can result in significant disruptions to essential health services. Pregnant women missed out on prenatal care, fewer babies were born in health care facilities, infants and children missed routine vaccinations, and emergency care was diminished – especially in places where health care workers were already in short supply.
In countries with high maternal and child mortality rates, such as Kenya, economic costs associated with these service disruptions and related higher non-COVID mortality represented a significant share of the overall economic burden. And when fear of infection causes health care workers to move into a less dangerous career or leave the workforce altogether, training replacements will require considerable time and money, compounding the problem of workforce shortages and driving the overall economic burden even higher.
3. Protecting health care workers now will save money and lives in the future
As countries continue to recover from the COVID-19 emergency, we must prioritize investments to build greater resilience in health systems, especially in lower-income countries. In particular, adopting even minimal improvements in infection prevention and control measures to protect health care workers will almost certainly avoid substantial costs in future epidemics and pandemics.
Thankfully, this needn’t be the case. Governments, with support from the international community, must take the lead in protecting health care workers as a global public good investment by:
- Collecting and analyzing high-quality data to accurately measure and report health care workers infections and deaths due to infectious diseases and using this knowledge to reduce risks to health care workers and their contacts.
- Taking accountability for protecting health care workers during infectious disease outbreaks. This includes implementing comprehensive infection prevention and control protocols and clean water, sanitation, and hygiene standards at every health care facility.
Although this study is limited in geographical scope and focuses on a single disease, it represents the first attempt to systematically estimate the economic burden of infection among health care workers – while also offering a framework for governments to quantify the return on investment for increased protections. These investments not only make economic sense – they are ethical imperatives for governments and funders to ensure we are better prepared for the next global threat.
Source : World Bank